Value in a Vial—Bortezomib for Injection from Baxter
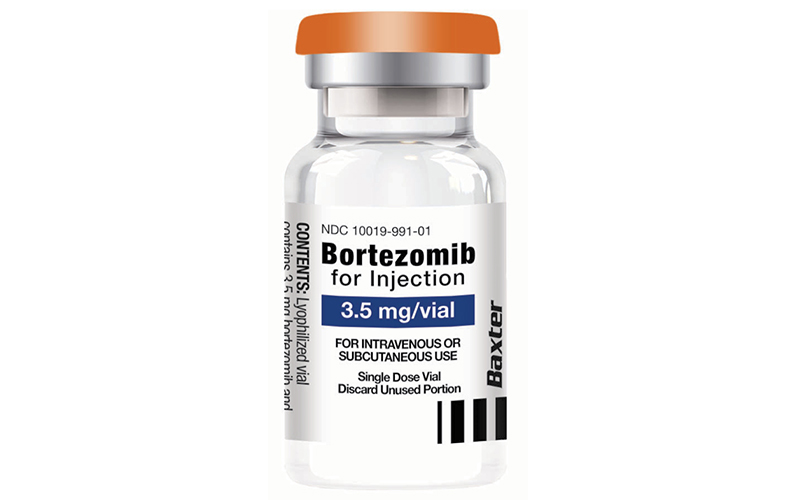
Bortezomib for Injection
Indications
Bortezomib for Injection is a proteasome inhibitor indicated for:
• treatment of adult patients with multiple myeloma
• treatment of adult patients with mantle cell lymphoma
Please read the accompanying full Indications and Important Risk Information and Prescribing Information.
Reliable supply, sustainable price, essential treatment for multiple myeloma and mantle cell lymphoma
Bortezomib for Injection from Baxter helps support patients with
• Part of the standard of care therapy for multiple myeloma and mantle cell lymphoma
• Consistent, reliable supply of Bortezomib from Baxter, a partner with the experience to support supply chain continuity
• A sustainable price backed by patient support programs
Order Bortezomib Now >
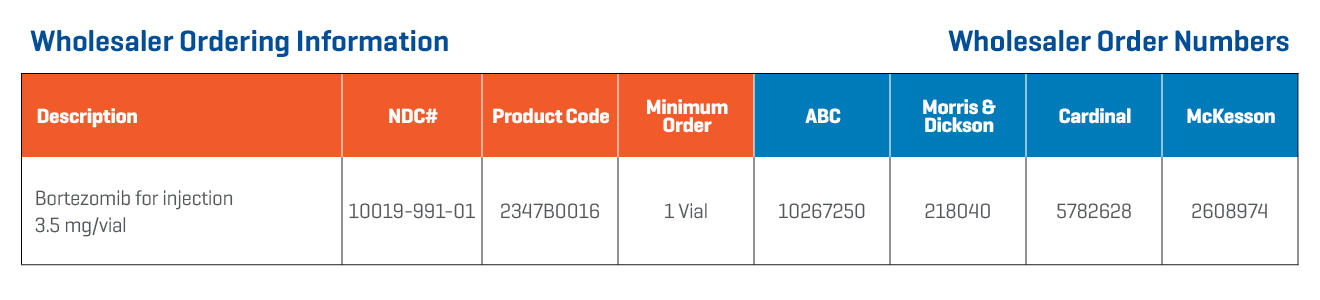
Baxter Bortezomib for Injection: Specifications
Indications and Important Risk Information
Indications
Bortezomib for Injection is a proteasome inhibitor indicated for:
• treatment of adult patients with multiple myeloma
• treatment of adult patients with mantle cell lymphoma
Important Risk Information
Contraindications
• Patients with hypersensitivity (not including local reactions) to bortezomib, boron, or mannitol. Reactions have included anaphylactic reactions.
• Contraindicated for intrathecal administration. Fatal events have occurred with intrathecal administration of Bortezomib for Injection.
Warnings and Precautions
• Peripheral Neuropathy: Bortezomib for Injection treatment causes a peripheral neuropathy that is predominantly sensory; however, cases of severe sensory and motor peripheral neuropathy have been reported. Patients with pre-existing symptoms (numbness, pain or a burning feeling in the feet or hands) and/or signs of peripheral neuropathy may experience worsening peripheral neuropathy (including ≥Grade 3) during treatment. Patients should be monitored for symptoms of neuropathy. Starting Bortezomib for Injection subcutaneously may be considered for patients with pre-existing or at high risk of peripheral neuropathy. Patients experiencing new or worsening peripheral neuropathy during therapy may require a decrease in the dose and/or a less dose-intense schedule. The long-term outcome of peripheral neuropathy has not been studied in mantle cell lymphoma.
• Hypotension: The incidence of hypotension (postural, orthostatic, and hypotension NOS) was 8%. These events are observed throughout therapy. Patients with a history of syncope, patients receiving medications known to be associated with hypotension, and patients who are dehydrated may be at increased risk of hypotension. Management of orthostatic/postural hypotension may include adjustment of antihypertensive medications, hydration, and administration of mineralocorticoids and/or sympathomimetics.
• Cardiac Toxicity: Acute development or exacerbation of congestive heart failure and new onset of decreased left ventricular ejection fraction have occurred during Bortezomib for Injection therapy, including reports in patients with no risk factors for decreased left ventricular ejection fraction. Patients with risk factors for, or existing heart disease should be frequently monitored. There have been isolated cases of QT-interval prolongation in clinical studies; causality has not been established.
• Pulmonary Toxicity: Acute Respiratory Distress Syndrome (ARDS) and acute diffuse infiltrative pulmonary disease of unknown etiology such as pneumonitis, interstitial pneumonia, lung infiltration have occurred in patients. Some of these events have been fatal. There have been reports of pulmonary hypertension associated with Bortezomib for Injection administration in the absence of left heart failure or significant pulmonary disease. In the event of new or worsening cardiopulmonary symptoms, consider interrupting Bortezomib for Injection until a prompt and comprehensive diagnostic evaluation is conducted.
• Posterior Reversible Encephalopathy Syndrome (PRES): PRES has occurred in patients receiving Bortezomib for Injection. PRES is a rare, reversible, neurological disorder which can present with seizure, hypertension, headache, lethargy, confusion, blindness, and other visual and neurological disturbances. Brain imaging, preferably MRI (Magnetic Resonance Imaging), is used to confirm the diagnosis. In patients developing PRES, discontinue Bortezomib for Injection. The safety of reinitiating therapy in patients previously experiencing PRES is not known.
• Gastrointestinal Toxicity: Bortezomib for Injection treatment can cause nausea, diarrhea, constipation, and vomiting sometimes requiring use of antiemetic and antidiarrheal medications. Ileus can occur. Fluid and electrolyte replacement should be administered to prevent dehydration. Interrupt Bortezomib for Injection for severe symptoms.
• Thrombocytopenia/Neutropenia: Bortezomib for Injection is associated with thrombocytopenia and neutropenia that follow a cyclical pattern with nadirs occurring following the last dose of each cycle and typically recovering prior to initiation of the subsequent cycle. The cyclical pattern of platelet and neutrophil decreases and recovery remain consistent in the studies of multiple myeloma and mantle cell lymphoma, with no evidence of cumulative thrombocytopenia or neutropenia in the treatment regimens studied. Monitor complete blood counts (CBC) frequently during treatment. Measure platelet counts prior to each dose of Bortezomib for Injection. Adjust dose/schedule for thrombocytopenia. Gastrointestinal and intracerebral hemorrhage has occurred during thrombocytopenia in association with Bortezomib for Injection. Support with transfusions and supportive care, according to published guidelines.
• Tumor Lysis Syndrome: Tumor lysis syndrome has been reported with Bortezomib for Injection therapy. Patients at risk are those with high tumor burden prior to treatment. Monitor patients closely and take appropriate precautions.
• Hepatic Toxicity: Cases of acute liver failure have been reported in patients receiving multiple concomitant medications and with serious underlying medical conditions. Other reported hepatic reactions include hepatitis, increases in liver enzymes, and hyperbilirubinemia. Interrupt Bortezomib for Injection therapy to assess reversibility. There is limited rechallenge information in these patients. Reduce the starting dose in patients with moderate or severe hepatic impairment.
• Thrombotic Microangiopathy: Cases, sometimes fatal, of thrombotic microangiopathy, including thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS), have been reported in the postmarketing setting in patients who received Bortezomib for Injection. Monitor for signs and symptoms of TTP/HUS. If the diagnosis is suspected, stop Bortezomib for Injection and evaluate. If the diagnosis of TTP/HUS is excluded, consider restarting Bortezomib for Injection. The safety of reinitiating therapy in patients previously experiencing TTP/HUS is not known.
• Embryo-Fetal Toxicity: Based on the mechanism of action and findings in animals, Bortezomib for Injection can cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to use effective contraception during treatment and for seven months following treatment. Advise males with female partners of reproductive potential to use effective contraception during treatment and for four months following treatment. If Bortezomib for Injection is used during pregnancy or if the patient becomes pregnant during treatment, the patient should be apprised of the potential risk to the fetus.
• Patients with Diabetes: During clinical trials, hypoglycemia and hyperglycemia were reported in diabetic patients receiving oral hypoglycemics. Patients on oral antidiabetic agents receiving Bortezomib for Injection treatment may require close monitoring of their blood glucose levels and adjustment of the dose of their antidiabetic medication.
• Adverse Reactions: Most commonly reported adverse reactions (incidence ≥20%) in clinical studies include nausea, diarrhea, thrombocytopenia, neutropenia, peripheral neuropathy, fatigue, neuralgia, anemia, leukopenia, constipation, vomiting, lymphopenia, rash, pyrexia, and anorexia.
• Drug Interactions:
• Strong CYP3A4 Inhibitors: Coadministration with a strong CYP3A4 inhibitor increases the exposure of bortezomib. Closely monitor patients with concomitant use.
• Strong CYP3A4 Inducers Coadministration with a strong CYP3A4 inducer decreases the exposure of bortezomib. Avoid concomitant use.
Please see accompanying full Prescribing Information for Bortezomib for Injection.